If you created a database of everything I’ve ever written, from the moment I first understood English to each school project to the advent of this column, I know exactly which word would appear the most often.
Diabetes.
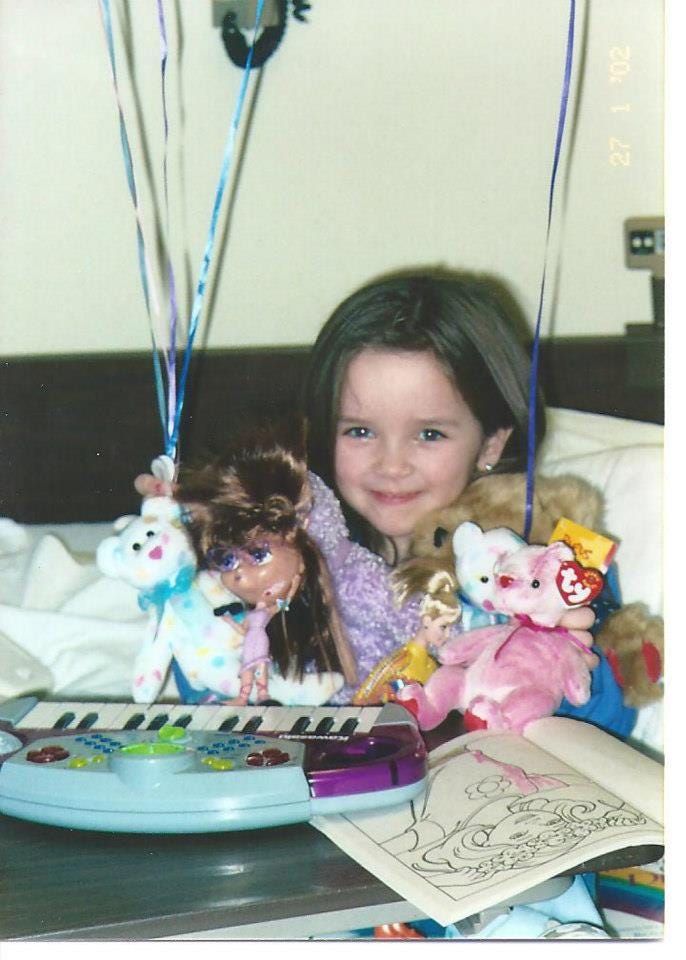
They say to write what you know, and there is no subject I know more intimately than Diabetes. Diagnosed at age 5, Type 1 Diabetes is the spilled nail polish that won’t come out of the carpet — it is stubborn, a huge bummer, and has seeped into every fiber of my life.
November is Diabetes Awareness Month, with November 14th being World Diabetes Day. I’ve lived with this disease for almost 22 years. Technology has evolved, costs have skyrocketed, health outcomes have improved, but each November comes and one thing never seems to change: the general public really does not understand this disease.
So each year, I take this month to share the intricacies of living without the function of a vital organ, in hopes that one day I will no longer have to.
But until then, here’s seven things I wish you knew about living with Type 1 Diabetes.
1. It can strike at any age
Diabetes has been through many different iterations of names; madhumeha (honey urine in ancient Indian language), the sugars, the sugar disease. The one you’ve probably heard of? Juvenile Diabetes.
But this was a misnomer. Even though Type 1 Diabetes is diagnosed most often in children, any person at any age can develop the disease. I know someone who was diagnosed when he was 6 months old, someone who was diagnosed when he was 13, someone who was diagnosed when she was 22, and someone who was diagnosed when she was 45. When people develop Type 1 Diabetes when they are older, they’re symptoms are often ignored, attributed to other illnesses, or diagnosed as Type 2 Diabetes. This lack of diagnosis can be detrimental, and often fatal.
I once had a school nurse ask me if the person we knew who was diagnosed at age 19 was “considered type 1 or type 2 due to her age,” and I swear I almost lost my mind.
And please, if you learn that someone has Type 1 Diabetes, DO NOT ASK THEM IF THEY WERE BORN WITH IT.
2. Type 1 and 2 are incredibly different diseases, but each with their own challenges
Type 1 Diabetes is an autoimmune disease in which the beta-cells in the pancreas are damaged, stopping the production of insulin and leading to hyperglycemia (high blood sugar levels). It cannot be cured or reversed; it can be managed with insulin therapy and blood sugar monitoring.
Type 2 Diabetes is a chronic metabolic disorder characterized by either a reduction in insulin production, an inability for the body to use insulin properly, or both. This is often diagnosed in older people and overweight people. However, it can also be genetic and have nothing to do with lifestyle. It can be managed with improved diet, exercise, medication, and blood sugar monitoring. Many Type 2 Diabetes require insulin, but not all and often not as aggressively as people with Type 1.
While related, these diseases are incredibly different and require incredibly different care regimens. It’s incredibly frustrating to have your disease consistently misunderstood and hear misinformation about how you should be caring for yourself.
Also, if you’re already aware of this difference, don’t fall into the trap of assuming one is “better” or “worse” than the other. Many people with Type 2 Diabetes are blamed and shamed in unhelpful ways. They experience fatphobia and are not taken seriously by the medical establishment. We all experience difficulties because of our Diabetes, no matter the type.
3. Everything affects my blood sugar. Literally. Everything.
People with Type 1 Diabetes make an extra 180 health-related decisions a day as compared to someone without Diabetes. This disease is fickle. People often assume that food is the main factor in changing blood glucose levels, but that couldn’t be further from the case.
The weather. My hormones. My mental health. Activity levels. The type of exercise I’m doing (aerobic and anaerobic exercise have two completely different effects). Stress. The amount of time that’s passed since I last put a new pump site in. Other medications. Other illnesses. Hydration levels. Alcohol. Whether or not my insulin has gone bad. How busy I am at work. Whether I take a hot shower or a cold shower. A change in routine.
All of these things affect how I decide to care for my disease.
It’s not just about food.
I consider this disease with every single choice I make. Leaving the house to drive down the street to the store? Make sure you have sugar with you in case you go low. Going on a trip? Take enough pump supplies with you for the week, then add four extras in case something goes wrong. Eating dinner? Make sure you know what your day will be like tomorrow so you dinner insulin sets you up for success.
A few years ago, I wrote up how I make decisions around working out. I have since changed to working out at 5:30 am, because having no active insulin before my workout takes out some of the variables that affect if I can workout or not.




Tired? Me too.
4. Insulin is not the only thing that costs too much for diabetes
People are often surprised when I tell them that insulin is one of the cheapest things I pay for with my diabetes.
Insulin is the base of the “Diabetic’s Hierarchy of Needs” and necessary to keep us alive, but the additional technology is what helps us thrive.
Insulin pumps allow for more precision in our insulin therapy and give us greater control over our blood sugars. My insulin pump is out of warranty and I’m purchasing a new one this month. Without insurance, it costs $5,500. With insurance and after my deductible, it’s $1,200. What happens if you don’t have an extra grand lying around?
When you have an insulin pump, you have to purchase pump sites, cartridges, tape to keep your site on, a case, a back up case for when your original one breaks. Alcohol wipes to clean your skin. Syringes in case your pump fails. Insulin pens if you don’t use a pump. Continuous glucose monitors that allow us to more closely monitor our blood sugar ranges - and the tape and skin tack that keeps those stuck to our bodies. The CGM transmitter. Blood glucose meters for back ups. Test strips. Emergency glucagon kits for bad low blood sugars. Low blood sugar snacks. Storage for your supplies. Bags to keep it on your person at all times.
Every one out of four healthcare dollars is spent on Diabetes in the U.S. The total annual cost of Diabetes in 2022 was $412.9 billion. We’re hurting.
5. PRICE CAPS AND COPAY CAPS ARE NOT THE SAME
There are a myriad of (evil) interests invested in the general public believing that progress has been made in making insulin more affordable. If you learn anything from me, please please please know: it hasn’t.
The confusion lies in copay caps vs. price caps. We’ve seen some legislation pass that limits how much can be charged as a copay for insulin. This is often $35.
My copay for insulin has been $35 for years.
The worry is not for me, someone who has never been without health insurance and will have support if I ever do lose it. It’s for those under- and uninsured, who are forced to pay thousands for this medication that they will die in days if they can’t access. Those people who lose their jobs out of nowhere and no longer have insurance. Copay caps will do nothing for them when they are forced to ration their insulin. Many of these copay caps are often only applicable to state-provided insurance, leaving millions more without these protections. Until we have justice in insulin price for ALL, we don’t have any.
Fight for price caps.
6. Be skeptical of the popular Diabetes nonprofits
Very few organizations that purport to protect and advocate for people with Diabetes actually do. Namely, JDRF and Beyond Type 1. These organizations take money from pharmaceutical companies that make insulin while refusing to disclose their funders. They have directly advocated against efforts to reduce the price of insulin. They have funneled money away from efforts to find a cure for Type 1 Diabetes and into technology that only the privileged will be able to afford..
For these organizations, money means more than our lives.
On a related note — Dexcom chooses to spend millions of dollars to put Nick Jonas in their commercials to market a continuous glucose monitor that every person with Diabetes is aware of and is actively prescribed to most people with Diabetes. A box of 3 Dexcom sensors costs me $330 and a Dexcom transmitter costs me $263. You couldn’t use that money to make your life-saving product a liiiiitle bit cheaper?!
7. Community is life saving for people with Diabetes
If you meet anyone with Type 1 Diabetes, no matter they’re age, I beg you to tell them about Camp Hertko Hollow.
If you’re new to this column, Camp Hertko Hollow is a camp for kids with Diabetes. I attended this camp for nine summers as a kid and have been volunteering as a counselor for seven. My husband, Matt, began attending the camp when he was six and is now the Programs Manager. This place has meant the world to our family.
Camp Hertko Hollow normalized my Diabetes for me. It transformed my relationship to my disease from something terrible that happened to me to a way of living my life. It gave me answers to every question and a space to make mistakes. I grew up knowing that camp, and it’s people, would forever be a constant in my life. It’s made me see Diabetes as an opportunity, and I want that for everyone.
Camp is for children age 6-17 to see others like them and learn about their disease. We are also always accepting volunteers, whether that be people with Diabetes or medical staff looking to learn more. It is a week filled with joy, learning, family, and the purest love you could imagine. Please, help us spread the word so everyone can have this experience.
The Iowa Writers Collaborative is hosting a holiday party for paid subscribers on Thursday, December 7th in Des Moines at the Witmer House. The Witmer House was once Iowa’s governor’s mansion and headquarters of the Iowa Girls High School Athletic Union. It’s a great opportunity to immerse yourself in Iowa history and meet writers from around our state. You can register here.
The Midwest Creative is a proud member of the Iowa Writers Collaborative. Please consider a subscription to my colleagues’ work to support storytelling across the state of Iowa. All of these authors provide content for free, with paid subscription options. Pick one or more, and help sustain this movement.




I wonder how many kids, teens, parents, relatives, that you’ve helped with everything you put out there about diabetes education?! Keep sharing and educating! I’m so proud of you 💙
Thank you Macey for sharing a personal insider view of diabetes. My wife coped with diabetes for 20 years, very costly. Not sure why insulin pens should have ncreased in price - what has changed? Manufacturing cost should have decreased using automation. T
hanks again - your words will have an impact on families and anyone involved in research for new treatments.